
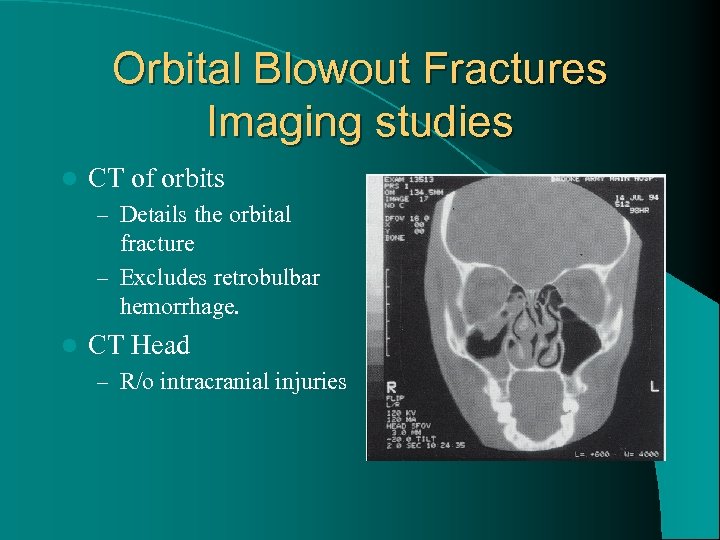
Frontal bone trauma at the brow may rarely transmit forces directly to the optic nerve without obvious fractures. An afferent pupillary defect may be seen in patients with fractures that extend into the optic canal or in cases of traumatic optic neuropathy or other types of eye trauma. Nasoethmoidal fractures can also cause damage to the lacrimal system and predispose patients to epiphora. Canthal dystopia may be seen at the lateral commissure in zygomatic fractures and at the medial commissure in nasoethmoidal fractures. Anesthesia in the distribution of the infraorbital nerve (including the lower eyelid, cheek, upper lip, and gums on the affected side) is common because most inferior orbital wall fractures are adjacent to the infraorbital neovascular bundle. Dysmotility and globe displacement can lead to diplopia in different directions of gaze. Often, enophthalmos is not present in the acute setting due to edema, hemorrhage, or both, and exophthalmometry may even show exophthalmos. Exophthalmometry measurements may show enophthalmos on the side of the fracture with large orbital wall fractures increasing the orbital volume ( Fig. Inferior displacement of the globe may be seen after a large inferior orbital wall fracture. In cases of entrapped orbital tissue, a surgeon should rely on direct visualization of the fracture site and not forced duction testing as evidence of release of tissue incarceration.Īsymmetry of globe positioning may be noted both initially and subsequently after orbital swelling has improved. We advocate forced duction testing only on a limited basis, under anesthesia if possible, and only if the findings will significantly change clinical or surgical management. Additionally, forced ductions are extremely uncomfortable with a patient who is awake. Forced duction testing, however, may be misleading in the acute post trauma setting due to hemorrhage and edema. Once the globe is deemed intact and stable, some advocate forced duction testing in the assessment of eye movement problems. Although radiographic imaging can be used to evaluate for muscle involvement, muscle entrapment is a clinical diagnosis. Posttraumatic dysmotility may also ensue from direct muscle damage or edema and nerve damage. Orbital tissue edema and muscle entrapment are common etiologies as is the loss of wall support ( Table 2 Figs. Restricted extraocular muscle movements may be present due to multiple mechanisms. Point tenderness or step-offs along the orbital rim may be noted in the location of a possible fracture involving the orbital rim. Crepitus may be noted if air from the sinuses has tracked into the subcutaneous tissues after nose blowing or sneezing. Varying degrees of periorbital ecchymosis and edema are typical after trauma. There are several common clinical exam findings, regardless of the etiology of the fractures, suggestive of an orbital fracture ( Table 1). Coronal computed tomography images of the obits showing a left inferior orbital wall fracture ( A) and irregularity of the nasal globe contour of the left eye ( B) suggesting a globe rupture.


 0 kommentar(er)
0 kommentar(er)
